How virtual technology developed by Cambridge University Hospitals ‘will help save babies’ lives’
Cambridge University Hospitals has developed virtual technology that effectively ‘parachutes’ its consultants into other hospitals in the region to help fellow medics care for seriously ill babies.
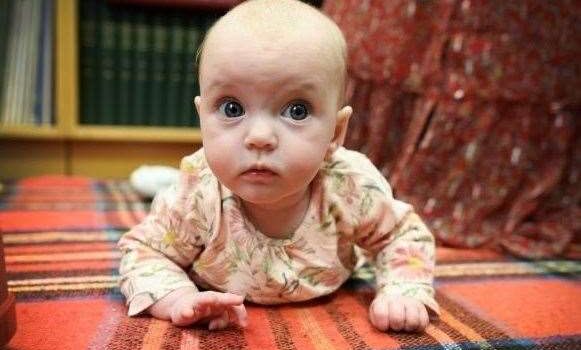
Aurelia Hunt was one of the first babies to benefit from this UK first when she became seriously ill with a suspected meningitis and sepsis infection after being born prematurely at Colchester Hospital.
Instead of being transferred for treatment to Addenbrooke’s in Cambridge, Aurelia was safely cared for in Colchester and her family were able to stay together.
The cloud-based technology platform, called LocANTS, enables consultants in Cambridge to monitor babies remotely - reading their notes, examining scans and X-rays, and checking readings from ventilators, infusion pumps and other equipment.
It has been in development since 2017 driven by Addenbrooke’s deputy medical director, Dr Sue Broster, paediatrician Dr Arun Dhar and London-based entrepreneur and IT consultant Ranadip Chatterjee.
The consultants - part of the Paediatric and Neonatal Decision Support and Retrieval Service (PaNDR) - can control cameras and microphones fitted to workstations in other neonatal units across the region to help doctors with tough decisions.
Dr Dhar, who devised the original concept, said: “Although it has been a long time in the making, and we have drawn on the expertise of a great many people, it is absolutely worth it because LocANTS will undoubtedly save lives.
“Our specialist PaNDR consultants will be able to access systems at work, at home, or anywhere else they can use their laptops. Ultimately, we hope to offer this service for children up to 16.”
The livestreamed data from each baby is monitored in the PaNDR control room in Cambridge. If a baby's condition deteriorates, the team can quickly transfer the baby by ambulance to a more specialised neonatal critical care unit, such as the one at Addenbrooke’s.
The system - previously shortlisted for a Cambridge Independent Science and Technology Award - means more babies can be treated closer to home, freeing up paediatric and neonatal ambulance crews and critical care cots for the sickest babies.
For Aurelia’s father, James Hunt, it was a great help.
"It was a huge relief that the technology existed. Had it been different, it would have completely blown our family life for a couple weeks,” he said. "It was hard enough already and it would have made it even harder."
Cambridge University Hospitals, which runs Addenbrooke’s and the Rosie maternity hospital, are trialling LocANTS at Peterborough, Colchester and Ipswich hospitals. If it is a success, it could be rolled out across all Eastern region, before making a bid to the NHS to implement it nationwide.
Dr Broster, a consultant in neonatal intensive care and neonatal transport medicine, said: “LocANTS now enables clinicians to pool their combined expertise to make difficult decisions about difficult cases in real time, even though they may be miles apart. It is in its infancy, but has the potential to become something very big.
“This is a classic example of different people, with widely differing skill sets, working as a team to develop something that has the potential to be truly remarkable and solve at a stroke a lot of risks, complications and pressures associated with neonatal transport.”
Support for the system was offered by Addenbrooke’s e-hospital team, particularly around digital governance, and further help came from the University of Cambridge Judge Business School, and the Eastern Academic Health Science Network, which is the innovation arm of the NHS.
Tthe NHS innovation support team, Health Tech Enterprise, formerly known as Health Enterprise East, also pitched in with a Medtech Accelerator award to aid its development.
Mr Chatterjee, a specialist in technical aspects of big data systems typically used for analytics, machine learning and AI, said: “I am delighted to be part of a project that levers and develops technology to create practical solutions to clinically and demographically challenging problems.
“I believe there is potential to develop LocANTS even further for the benefit of patients.”







Gloss